It does not typically cause a pinched nerve, but excessive or misdirected pressure over nerve pathways or narrowed foramina can aggravate existing compression. Neural irritation presents as sharp, electric, or distal tingling, weakness, or dermatomal numbness. Clinicians avoid perpendicular shear over superficial nerves and modulate pressure, angles, and joint position to protect neurovascular structures. Red flags include progressive weakness, night pain, saddle anesthesia, or bowel/bladder changes. Proper technique, screening, and aftercare reduce risk; details on safety and signs follow.
What a Pinched Nerve Is and How It Happens

A pinched nerve, medically termed nerve compression or entrapment, occurs when surrounding tissues—such as intervertebral discs, facet joints, muscles, tendons, or inflamed fascia—apply sustained pressure on a peripheral nerve or its root, disrupting normal signal conduction.
Common mechanisms include cervical or lumbar disc protrusion narrowing the intervertebral foramen, facet hypertrophy or osteophytes creating foraminal stenosis, and myofascial tightness compressing superficial branches. Inflammatory edema further reduces local glide, amplifying ischemia and ectopic firing.
Clinically, this presents as dermatomal pain, paresthesia, weakness, or diminished reflexes, depending on the level and duration of compression.
At Spa & Massage clinics in London, therapists recognise red flags—progressive weakness, severe night pain, bowel or bladder changes—and encourage prompt medical evaluation, while tailoring comfort-focused positioning to reduce mechanical provocation during any wellness session. Notably, athletes can benefit from sports massage techniques that help alleviate muscle tension and support healthy nerve function, potentially reducing the risk of nerve compression.
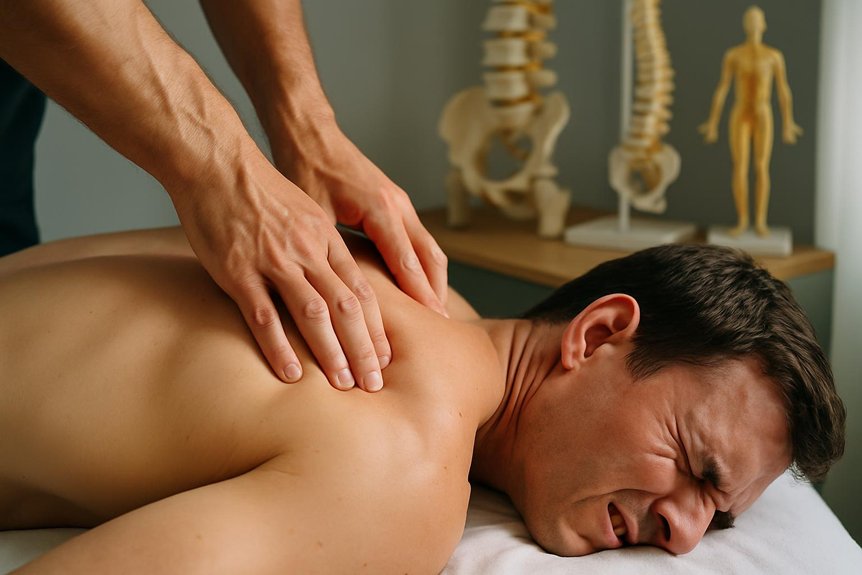
How Deep Tissue Massage Works on Muscles and Fascia
It targets layered muscle tension by applying graded pressure from superficial to deep fibers, following the direction of fascicles and avoiding neural structures. Sustained, slow strokes facilitate myofascial release by reducing cross-link adhesions within the fascia and improving glide between muscle compartments.
Focused ischemic compression and friction techniques are then used to deactivate trigger points, smoothing taut bands and normalizing local perfusion.
Layers of Muscle Tension
Within the musculoskeletal system, tension accumulates across stratified tissues—epidermis and superficial fascia, deeper myofascial layers, and contractile muscle fibers—each responding differently to pressure and shear.
In practice, precise assessment distinguishes cutaneous guarding from fascial densification and true myofibrillar hypertonicity. Superficial glide detects skin drag; slower, angled strokes test fascial compliance; sustained compression gauges muscle end-feel and trigger point referral.
At Spa & Massage clinics in London, therapists modulate depth and vector to meet the layer that is restricting movement, not simply press harder. Gentle warming strokes reduce nociceptive vigilance; then gradual sink allows contact with the myofascial envelope before addressing taut bands within specific muscle bellies.
Layer-by-layer pacing helps disperse adhesions, restore slide between tissues, and reduce nerve irritability from surrounding muscular tension.
Fascia Release Mechanics
Building on layer-specific assessment, fascia release focuses on restoring glide between collagen fibers and adjacent tissues through controlled load and time.
In practice, therapists at Spa & Massage apply slow, perpendicular or longitudinal shear with calibrated pressure, maintaining each contact until viscoelastic creep and thixotropic softening occur.
This reduces cross-link density, improves interstitial fluid exchange, and normalises sliding between epimysium, perimysium, and adjacent fascial planes.
Care is taken to angle strokes away from neurovascular trunks, minimising mechanosensitive nerve irritation.
Evidence suggests moderate, sustained pressure (60–90 seconds) modulates fibroblast tension via integrin signaling, enhancing tissue extensibility without provoking inflammatory flare.
In clinic, therapists monitor breath, tissue yield, and client-reported depth to titrate load.
The aim is quiet, unforced lengthening, restoring supple motion that feels safe and deeply relieving.
Trigger Point Smoothing
A focused approach to trigger point smoothing targets hyperirritable nodules within taut bands of skeletal muscle, typically at motor endplates. Practitioners at Spa & Massage apply slow, perpendicular compression followed by longitudinal gliding to reduce end-plate noise, normalize sarcomere length, and restore myofascial glide.
Pressure is titrated to a tolerable “good ache,” sustaining ischemic compression for 20–60 seconds until a softening or referred pain fade occurs.
Clinically, this downregulates nociceptive input via spinal gating, improves local perfusion, and interrupts sustained acetylcholine release.
Priority regions include upper trapezius, levator scapulae, piriformis, and quadratus lumborum—sites frequently implicated in pseudo-radicular pain.
Can This Trigger or Worsen a Pinched Nerve?
A pinched nerve is mechanical compression or irritation of a peripheral nerve root or peripheral nerve by adjacent structures such as herniated disc material, osteophytes, or hypertrophic soft tissue.
While it can reduce myofascial tension that contributes to secondary nerve irritation, excessive pressure or sustained compression over a compromised foramen or entrapment site may aggravate neuritic symptoms (sharp pain, paresthesia, motor weakness).
At Spa & Massage, therapists modulate pressure, avoid direct loading over suspected entrapment pathways, and adapt techniques immediately if neural symptoms are reproduced.
What a Pinched Nerve Is
Pinched nerve describes mechanical compression or irritation of a peripheral nerve or nerve root, typically from disc herniation, foraminal narrowing, osteophytes, swollen soft tissues, or tight myofascial structures. The result is impaired axonal conduction and local neuroinflammation, often felt as sharp, electric pain, tingling, numbness, or weakness along a dermatomal or peripheral nerve distribution.
In the neck, this may radiate into the arm; in the low back, into the leg. Focal entrapments—such as at the piriformis, scalene triangle, or carpal tunnel—produce predictable patterns.
Clinically, tenderness over entrapment sites, reduced reflexes, and myotomal weakness guide assessment.
At Spa & Massage, therapists recognise red flags and adapt pressure, positioning, and pacing to respect neural tissue sensitivity, supporting comfort while encouraging circulation and gentle mobility.
When Deep Pressure Backfires
Understanding that neural tissue can be mechanically sensitive, the next question is whether forceful techniques risk aggravation. Deep pressure can transiently increase intramuscular tension and local edema. Over vulnerable sites—cervical foramina, the scalene triangle, subacromial space, piriformis corridor, or lumbar paraspinals near facet joints—this may narrow neural passages and intensify radicular symptoms.
Excessive compression over a sensitized nerve trunk or inflamed root can provoke ectopic firing, after-sensation, and protective spasm.
From Spa & Massage’s clinical perspective, risk rises with high-load, sustained strokes applied without symptom monitoring, especially in acute disc irritation or nerve entrapment. Their therapists modulate load, biasing slower, melt-like pressure, nerve-sensitive positioning, and gliding that respects tissue yield.
Red flags—sharp, distal, electric pain or progressive numbness—prompt immediate pressure reduction and referral.
Signs You Should Pause or Modify a Session
When should a deep tissue session be paused or modified for someone with suspected nerve irritation? Clear red flags include sharp, electric pain radiating along a dermatome; distal tingling or numbness that persists beyond 30 seconds; new weakness in a myotomal pattern (e.g., grip giving way, foot drop sensation); increased allodynia or burning along a nerve path; or loss of two‑point discrimination compared with the other side.
Palpation over known entrapment sites—scalenes, pectoralis minor, pronator teres, piriformis, fibular head—provoking paresthesia also warrants adjustment. Escalating pain with neural tension positions (cervical side‑bend, slump, straight‑leg raise) is another cue.
At Spa & Massage, therapists reduce depth, switch to gentle fascial unloading, avoid end‑range compression, and document changes while encouraging immediate client feedback.
Techniques Our Therapists Use to Protect Nerves
How do skilled hands apply pressure without provoking neural irritation? At Spa & Massage, therapists map nerve pathways—ulnar at the medial elbow, sciatic beneath the piriformis, common peroneal at the fibular neck—and modulate depth to spare neural tissue. They begin with slow effleurage to assess glide, then layer-specific compression along muscle fibers, avoiding perpendicular shear over superficial nerves.
Palpation distinguishes taut band from nerve cord; tingling or electric pain cues immediate dose reduction. Joint positioning slackens vulnerable structures: hip external rotation to decompress the sciatic path, cervical side-bending to ease brachial plexus tension. Myofascial release lengthens fascial envelopes without compressive pinch.
In our clinics, hypoallergenic oils enable controlled drag. Therapists pace strokes to capillary refill, employ breath-synchronized pressure, and alternate work with lymphatic clears to minimise neurogenic inflammation.
Who Is at Higher Risk and When to Seek Medical Advice

Certain groups carry a higher likelihood of nerve compression: individuals with cervical or lumbar disc degeneration, foraminal stenosis, or osteophytes; those with diabetes, hypothyroidism, B12 deficiency, or inflammatory arthropathies; athletes with repetitive loading (runners: common peroneal; cyclists: ulnar at Guyon’s canal); workers with sustained flexion/extension or vibrational exposure; and people with recent trauma, edema, or postoperative scarring.
In Spa & Massage clinics, therapists screen for these factors and adapt pressure, angle, and duration to minimise neural irritation along entrapment sites such as the scalenes, piriformis, cubital tunnel, and tarsal tunnel.
Medical advice is warranted when weakness, dermatomal numbness, progressive paresthesia, night pain, saddle anaesthesia, bowel/bladder change, or unremitting radicular pain occurs.
New foot drop, grip loss, or post-massage burning along a specific nerve warrants urgent assessment. Therapists pause treatment and refer appropriately.
Safe Aftercare and Recovery Tips Following Therapeutic Deep Massage
Although deep tissue work can relieve myofascial tension around irritated neural pathways, ideal outcomes depend on structured aftercare that modulates tissue load and supports neural recovery.
At Spa & Massage, therapists recommend a 24–48 hour deload: avoid heavy lifting, high-intensity training, and end-range spinal loading. Gentle mobility—pain-free cervical rotations, thoracic openers, hip hinging—maintains glide of nerves and fascia without provoking symptoms.
Hydration and a light protein-rich meal support tissue perfusion and repair.
Clients may use brief, warm showers to promote vasodilation; ice is reserved only for acute, focal inflammation. Self-massage with a soft ball stays superficial, avoiding numb areas or radiating pain.
Sleep in neutral alignment with a supportive pillow. Red flags—progressive weakness, increasing numbness, or night pain—warrant medical assessment.
In follow-ups, our therapists titrate pressure, angles, and dosage to the individual response.
Conclusion
In closing, the clinic frames this therapy as tuning a guitar: precise tension yields resonance, excess twists a string. One review found only 0.7% of sessions led to transient neurological symptoms, underscoring low risk with skilled care. When therapists map dermatomes, palpate for myofascial trigger points, and modulate pressure along fascial lines, nerves glide rather than snag. A runner’s sciatic-like pain eased after graded hip rotator release—proof that informed technique clarifies, rather than clouds, neural pathways.













